Unlocking the Value of Combination Therapies


“If no action is taken - warns the UN Ad hoc Interagency Coordinating Group on Antimicrobial Resistance who released the report – drug-resistant diseases could cause 10 million deaths each year by 2050 and damage to the economy as catastrophic as the 2008-2009 global financial crisis. By 2030, antimicrobial resistance could force up to 24 million people into extreme poverty.”
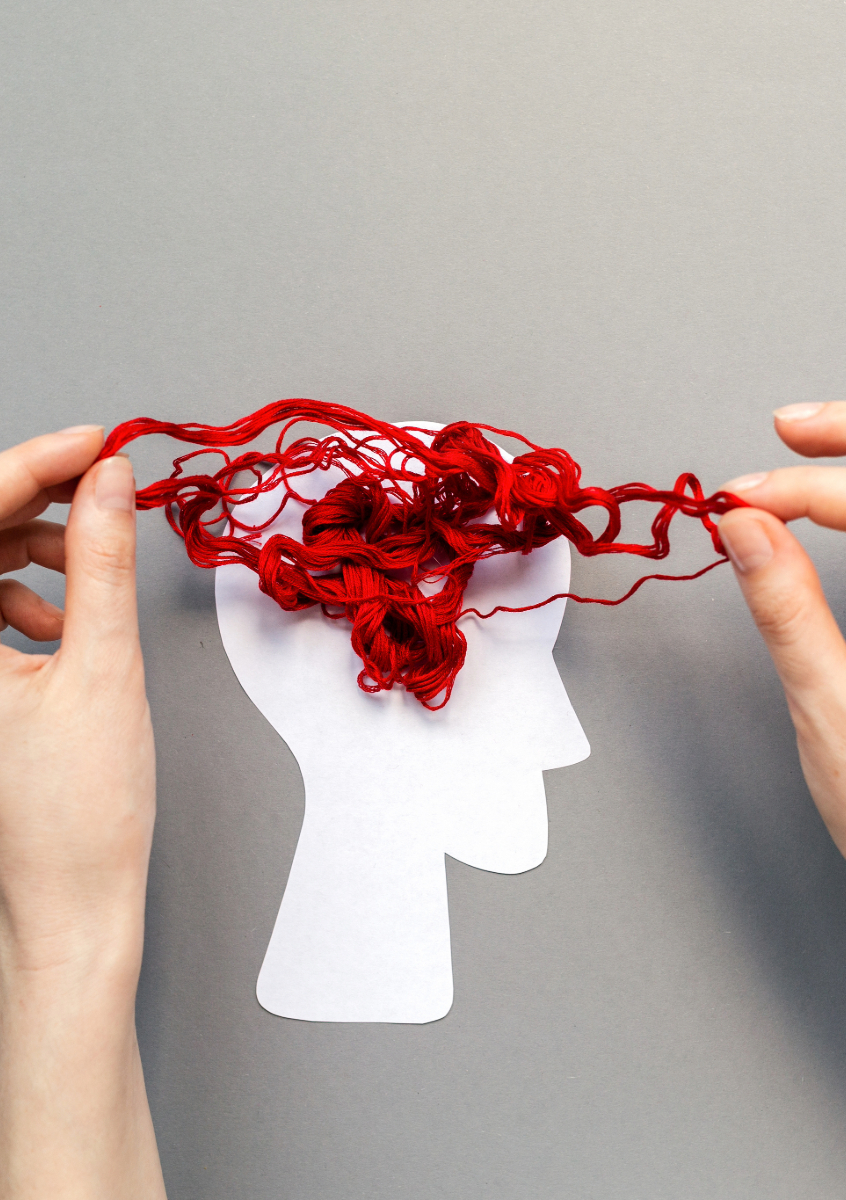
Antimicrobial Resistance (AMR) occurs when microorganisms such as bacteria, viruses, fungi, and parasites evolve, rendering medications ineffective. Overuse and misuse of antibiotics and antimicrobial drugs contribute to this global health threat, leading to infections that become increasingly difficult or impossible to treat, posing severe risks to public health.
AMR has been recognized as a pressing global threat, acknowledged by organizations like the World Health Organization (WHO) and the UN Ad hoc Interagency Coordinating Group on Antimicrobial Resistance. If left unaddressed, AMR could lead to dire consequences, projecting up to 10 million annual deaths by 2050 and a financial impact comparable to the 2008-2009 global financial crisis. The anticipated toll extends beyond mortality rates, as AMR may force around 24 million individuals into extreme poverty by 2030.
In Europe alone, AMR already poses a significant problem, contributing to approximately 670,000 infections and 33,000 fatalities annually due to resistant bacteria. Globally, the toll is staggering, with an estimated 1.27 million premature deaths attributed to AMR in 2019.
Health economics plays a crucial role in understanding the economic impact of AMR and devising strategies to address this global health threat. The financial burden of AMR on national economies is substantial, encompassing not only healthcare costs but also the loss of productivity among affected individuals and caregivers.
Health economists are exploring innovative approaches to incentivize investment in the development of new antibiotics. Among these approaches are “push incentives,” providing upfront funding for research and development (R&D), and “pull incentives,” which reward successful products upon market entry. These incentives aim to counter the economic disincentives that hinder antibiotic development due to the traditional volume-based sales model.
One proposed solution involves a subscription payment model similar to streaming services like Netflix. This model ensures developers receive rewards for novel antibiotics irrespective of sales volume, offering financial incentives independent of usage. This strategy aims to stimulate antibiotic R&D by providing adequate rewards, granting patient access to new antibiotics, and allowing healthcare systems to implement antimicrobial stewardship practices.
While several attempts have been made to establish subscription payment models, successful implementation remains limited. The UK has initiated a pilot project and plans to introduce a more permanent Netflix-style payment model. This innovative approach in healthcare financing aligns rewards with the societal value of novel antibiotics, addressing the economic challenges of antibiotic development while safeguarding their appropriate use to combat AMR. Continued exploration and adoption of such models by health economists and policymakers globally could catalyze antibiotic innovation and mitigate the threat posed by AMR.
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!