In this report, we propose a novel payment model that will incentivise broader value demonstration for diagnostics for antibiotics that could inform longer-term financing and reimbursement arrangements and guide prescribing behaviours.
Key takeaways
- Antimicrobial resistance (AMR) threatens our ability to treat common infections, and antibiotic stewardship is critical to curbing this global threat
- Appropriate use of (new) antibiotics relies on diagnostics, and efforts to incentivise antibiotic innovation will be wasted if incentives for diagnostics are overlooked
- These include poor incentives for high-value diagnostic innovation, low willingness to pay for AMR diagnostics from local budget holders, and low evidence of value at the point of adoption
- A novel payment model is proposed that will incentivise broader value demonstration to inform longer-term financing and reimbursement arrangements and guide prescribing behaviours
Antimicrobial resistance (AMR) is a global issue that threatens our ability to treat common infections and has large economic implications. Stewardship activities are needed to preserve antibiotics and reduce the rate of resistance. Diagnostics can support antibiotic stewardship by informing clinical decisions and reducing inappropriate antibiotic prescribing.
However, there is a range of challenges that limit their adoption at levels needed to support antibiotic stewardship. These include poor incentives for high-value diagnostic innovation, low willingness to pay for AMR diagnostics from local budget holders, lack of awareness, and low evidence of value at point of adoption.
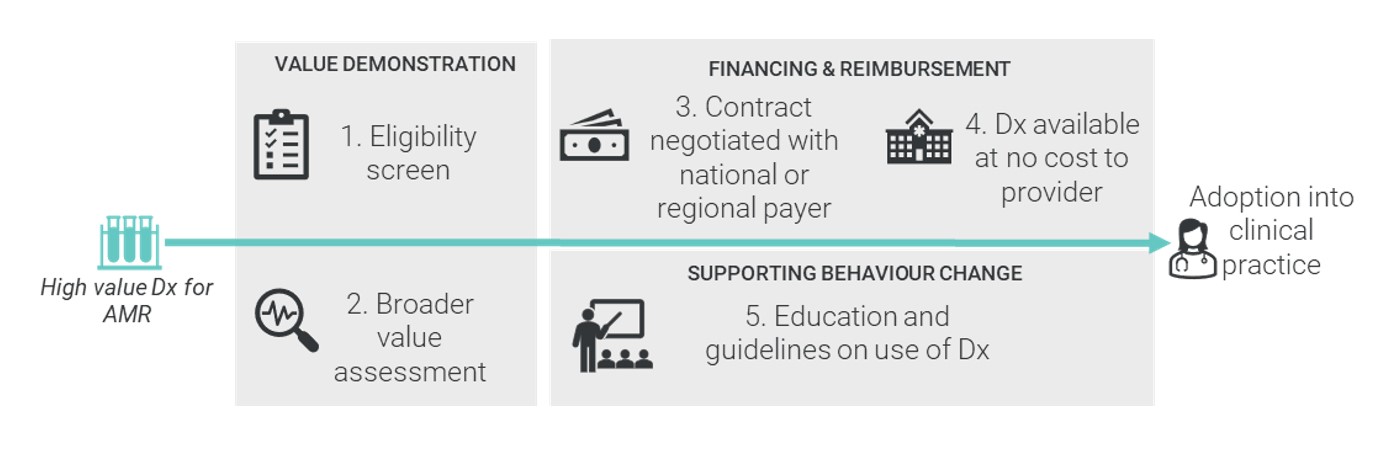
To address these challenges, a novel payment model is proposed to overcome these barriers. The payment model should have the following general design criteria:
- Procurement must be aggregated at a level above the individual provider such that providers are cost-neutral to the use of a diagnostic (i.e. using the diagnostic will not increase the cost of delivering care).
- The procurement level must be value-based, informed by a value assessment based on evidence of efficacy and value.
- The payment contract must be negotiated over multiple budget cycles to generate a form of exclusivity and revenue certainty for developers.
- Eligibility for the novel payment model is limited therefore not all diagnostics that could support antibiotic stewardship would automatically gain reimbursement through this mechanism.
- Eligibility criteria for the mechanism should be based on health system priorities set by payers and informed by international unmet need.
- The payment model must be accompanied by specific education and behaviour change initiatives to support the uptake of diagnostics reimbursed within the scheme.
This proposal should be supported in national AMR action plans and fitted into existing clinical education processes and incentive structures.
SCHEMATIC OF NOVEL INCENTIVE MODEL FOR DIAGNOSTICS (DX) THAT HELP TO COMBAT AMR
The vital attention that the economics of antibiotics is receiving, including initiatives such as the NICE-NHS England pilot in the UK and the PASTEUR Act in the US, is a moment of opportunity to redefine how health technologies with a large impact on global public health should be procured.
While these initiatives for antibiotic development are promising, addressing the antibiotic resistance crisis requires both development of new antibiotics and more appropriate use of existing ones.
Appropriate use of antibiotics relies on diagnostics, so the efforts taken to incentivise antibiotic innovation will be wasted if incentives for diagnostics are overlooked. Much has been said about the importance of diagnostics to the AMR crisis, but now is the time for policymakers to act.
This contract research report, ‘A Novel Incentive Model for Uptake of Diagnostics to Combat Antimicrobial Resistance’, was commissioned and funded by Roche Diagnostics.




