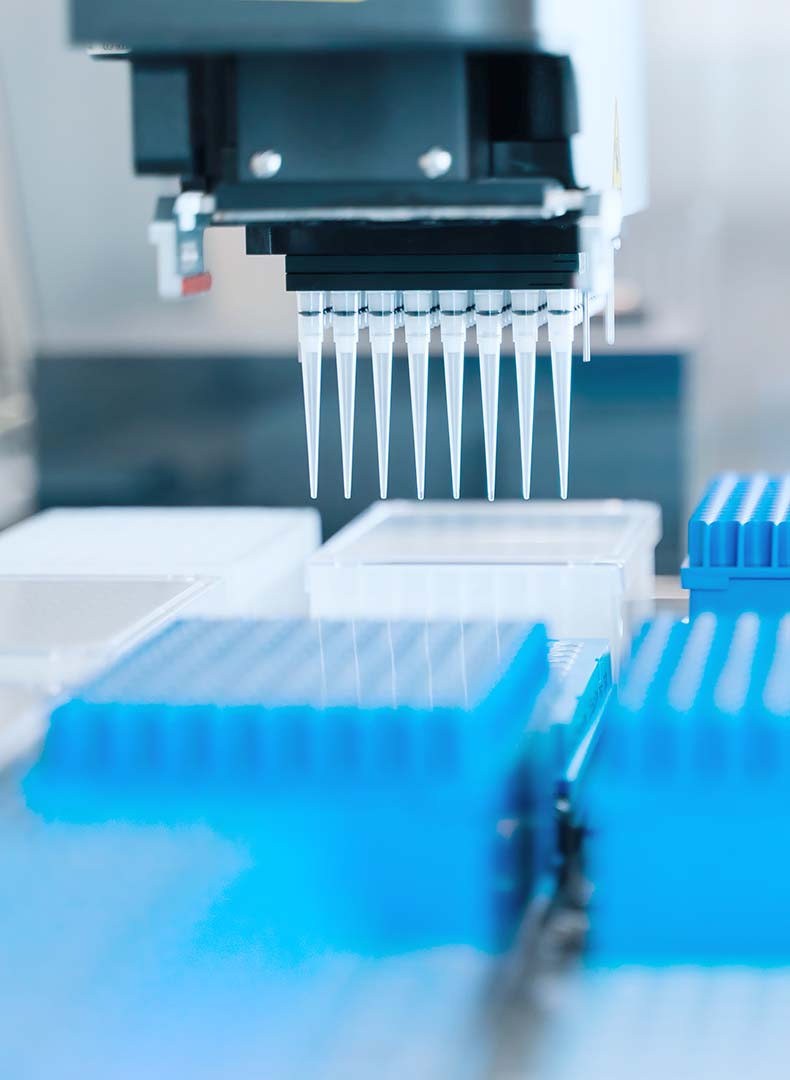
A Novel Incentive Model for Uptake of Diagnostics to Combat Antimicrobial Resistance

A new OHE report discusses NICE’s introduction of a cost-effectiveness threshold to appraise ultra-orphan drugs.
A new OHE Consulting Report has been published that discusses the use of a cost-per-QALY gained decision rule to appraise treatments for very rare conditions, as part of the NICE Highly Specialised Technologies (HSTs) programme.
The NICE HST programme started in 2013 and its interim method and process guide embraced a wide range of decision-making criteria to consider factors beyond direct health benefits captured by quality-adjusted life years (QALYs). Key changes to the HST method introduced from April 2017 are:
The OHE Report argues that:
Click here to download the full report.
For more information, contact Martina Garau.
Related OHE publications:
Zamora, B., Maignen, F., O’Neill, P., Mestre-Ferrandiz, J. and Garau, M. (2017). Comparing Access to Orphan Medicinal Products (OMPs) in the United Kingdom and other European countries. OHE Consulting report. London: Office of Health Economics.
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!