Unlocking the Value of Combination Therapies

Epilepsy is a chronic, neurological disorder characterised by spontaneous and recurrent seizures, which are a sudden onset of abnormal electrical activity in the brain that temporarily affects how it works. The most common ways of treating epilepsy are medicines called anti-seizure medications (ASMs), but research has found that some ASMs can harm an unborn baby if the mother is taking them during pregnancy. However, evidence regarding the risk profiles of many ASMs, including those recommended for use by the NHS, remains uncertain or limited to a subset of the potentially impacted conditions.
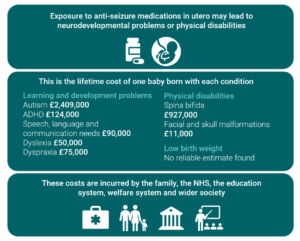
We aimed to quantify the economic impact associated with conditions that may have an increased risk as a result of exposure to ASMs. Due to limited information on ASM-specific risks, we were unable to estimate the number of cases of each condition attributable to ASMs or the proportion of total conditions costs attributable to ASMs.
Much of the research assessing the impact of ASMs on the risk of congenital conditions is based on studies that focus on, or include, valproate. The unacceptable risks associated with valproate are well-recognised and it is specifically discouraged for women of child-bearing age. Therefore, using risk estimates from studies that include valproate is likely to overestimate the ASM-attributable prevalence and impacts of these conditions. Instead, we estimate the lifetime cost per case of each condition to highlight the potential economic impact associated with in utero exposure to ASMs at the individual level.
We find that in utero exposure to ASMs has substantial consequences for affected individuals, their families, the NHS, other government sectors, and society as a whole. Our estimates of these costs range from £50,000 for dyslexia to almost £2.5 million in extreme cases of autism spectrum disorder.
Figure 1 Overview of lifetime cost per condition (to the nearest £1,000)
A substantial limitation of these cost estimates is our inability to extrapolate them to the population level on the basis of ASM-attributable risks due to an absence of such risk estimates in the literature. To address this limitation, we suggest collecting the following data:
Reliable assessment of the ASM-attributable economic impact can be used as a signal to guide research funding toward interventions that aim to reduce such impacts.
This research paper, ‘Individual, Health System, and Societal Impacts of Anti-seizure Medicine Use During Pregnancy’, was commissioned and funded by the Epilepsy Society.
Individual, Health System, and Societal Impacts of Anti-seizure Medicine Use During Pregnancy