Thrombosis had been recognised as a disease since around 2000 BC, but the word thrombosis was first used by Claudius Galenos (130 – 200 AD). Pulmonary…
Thrombosis had been recognised as a disease since around 2000 BC, but the word thrombosis was first used by Claudius Galenos (130 – 200 AD). Pulmonary embolism was described for the first time by Wiseman in 1676 but the relationship between venous thrombosis…
Thrombosis had been recognised as a disease since around 2000 BC, but the word thrombosis was first used by Claudius Galenos (130 – 200 AD). Pulmonary embolism was described for the first time by Wiseman in 1676 but the relationship between venous thrombosis and pulmonary embolism was not clarified until the 1840s by Rudolf Virchow. In 1856 Virchow described a triad for the origin of thrombosis which remains valid today. He suggested that blood stasis, injury to the blood vessel wall and alteration of the blood constituents are the main causes of venous thrombosis. Although much has occurred in thrombosis research in the past 150 years, the investigation of the mechanism by which it arises is still focussed on blood flow conditions, on changes in the vessel walls, and on the properties of blood. It is now generally recognised that one factor alone is not usually sufficient to produce a thrombus. For example, stasis during normal sleep or bed rest in the absence of other risk factors will not usually cause a thrombus.
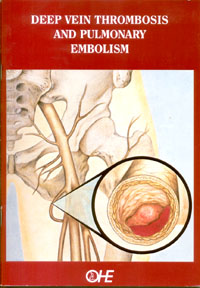
Although thrombosis has been described in a variety of anatomic sites, the most common and clinically significant are the deep veins of the legs. Venous thrombi occur in regions of slow blood flow, where local activation of blood coagulation by a variety of thrombogenic stimuli results in the formation of small deposits of fibrin. These deposits often originate within the deep veins of the calf or thigh and may serve as the starting point for thrombus growth, with subsequent entrapment of blood cells and formation of additional fibrin gel. If the evolving thrombus extends proximally and grows large enough to cause obstruction to venous outflow the patient may experience pain and swelling in the affected limb. Alternatively if the thrombus dislodges and travels upwards the result may be pulmonary embolism (Millensen & Bauer, 1996).
Thrombosis as a complication following surgical operations was reported for the first time in 1894 by von Strauch. Pulmonary embolism as an important postoperative cause of death began to attract attention around the turn of the century. In 1905, a survey among different surgeons in the United States demonstrated that patients who underwent operations in the lower part of the abdomen and/or gynaecological surgery were at high risk of developing a postoperative thrombosis (Cordier, 1905). Lister (1927), in an analysis of the then current state of knowledge, observed that advancing age was an important risk factor for the development of post-traumatic pulmonary embolism. At about the same time Gustat Petren made an analysis of the causes of postoperative mortality and deaths from pulmonary embolism, their increased number and our, in the main, helplessness in the face of them, both prophylactically and therapeutically, make pulmonary embolism the greatest crux of present day practical surgery’.
Unfortunately, although our knowledge of the causes of deep vein thrombosis and the therapeutic and prophylactic measures available to treat and prevent venous thromboembolic diseases have increased, it continues to be of great importance in surgery today and is still a major cause of postoperative death.
This paper sets out what is currently known about venous thromboembolic diseases:
• describes the incidence and prevalence of the condition;
• discusses the associated risk factors and their relative importance;
• relates the difficulties that exist in making an accurate diagnosis of deep vein thrombosis;
• considers the regimens which exist to both treat and prevent deep vein thrombosis and their relative cost effectiveness using published economic evaluations;
• looks at the cost to the NHS of deep vein thrombosis in 1993/94 and calculates the potential costs and lives saved if adequate prophylaxis had been used; and
• concludes by asking what might be done to ensure that all patients at risk of developing a deep vein thrombosis receive adequate prophylaxis.