The report highlights the burden of Hidradenitis Suppurativa (HS) on patients, the NHS and society and makes recommendations to improve life for people living with HS and lessen the burden on the NHS and wider society. The foreword has been provided by Angela Gibbons, patient and HS advocate. This project has been organised and funded by Novartis Pharmaceuticals UK Ltd, with support from M+F Health. The report is informed by input from experts working in HS, including leading clinicians.
Key takeaways
- Hidradenitis Suppurativa (HS) is a painful chronic skin disease estimated to affect at least 200,000 people in the United Kingdom. It is debilitating condition that can have a significant impact on emotional well-being and quality of life.
- Currently, there is no cure for HS; existing treatments primarily focus on wound and pain management. Furthermore, awareness of the condition is low among the general public, and it is under-recognised by primary care physicians, leading to a significant diagnostic delay.
- People with HS face an average diagnostic delay of 10 years, and over 70% of patients are already exhibiting moderate to severe disease when first diagnosed. This, in turn, can have a significant impact on mental health, with depression and anxiety twice as common in people with HS than in the general population.
- Our economic analysis estimates that the annual monetary impact of HS in the UK is around £3.83 billion, based on the resource utilisation costs directly associated with HS and its associated comorbidities to the NHS, out-of-pocket costs to people living with HS, and productivity losses to wider society.
Hidradenitis Suppurativa (HS) has a significant impact on the wellbeing of people living with the condition, the National Health Service (NHS), and broader society, but HS and its range of impacts are not well recognised. In this report, we seek to identify and quantify the humanistic and socioeconomic burdens of HS in the United Kingdom. We shed light on different dimensions of HS, including its impact on individuals and families, and the healthcare system, as well as the broader societal consequences of this poorly understood and often misunderstood condition.
People living with HS experience a major impact on their quality of life, with physical pain, poor mental health, and social isolation among the biggest burdens. Wound management incurs considerable costs in terms of time and money, with most patients requiring 1-3 dressing changes per day. HS also impacts social and intimate relationships, education, and employment prospects.
A relative lack of awareness among affected people and physicians can lead to delayed diagnoses and misdiagnoses, meaning that many patients are exhibiting moderate to severe disease by the time they get diagnosed. HS is also associated with a range of comorbidities, the most prevalent of which include cardiovascular disease, hypertension, obesity, and diabetes. Furthermore, there is a shortage of dermatologists, specialist nurses and psychodermatology practitioners in the NHS. This combination of factors leads to avoidable burdens for the NHS and people with HS, in terms of direct healthcare costs and health outcomes.
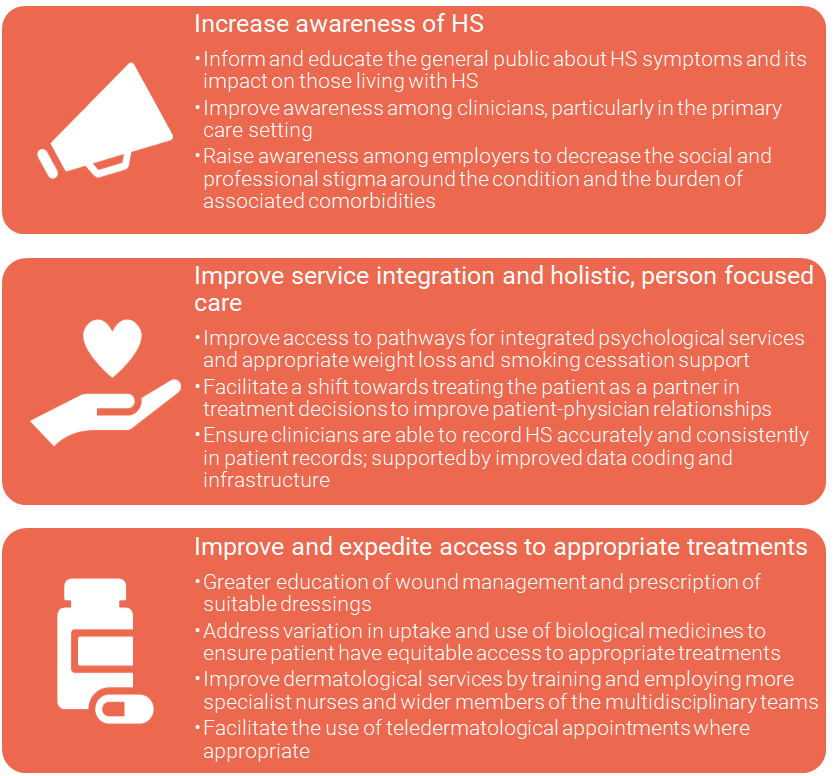
We propose three recommendations to improve life for people living with HS and lessen the burden on the NHS and wider society based on our research and input from our patient and clinician focus group.
Key Recommendations:
This consulting report. ‘The Burden of Hidradenitis Suppurativa on Patients, the NHS and Society’, was commissioned and funded by M&F Health on behalf of Novartis.



