Antimicrobial Resistance (AMR)
The WHO lists AMR in the top 10 global health threats but new antibiotic development is not keeping pace with the emergence of resistant pathogens. Novel ways to structure the market are being explored which incentivise developers and give healthcare systems new tools to fight AMR.

An Insurance Framework for Funding New Antibiotics
22 September 2017
A new paper sets out an insurance model as part of a global solution to incentivise R&D for new antibiotics to tackle multi-drug resistance. It offers…

Assessing the Value of New Antibiotics: Additional Elements of Value for Health Technology Assessment Decisions
30 May 2017
Without new antibiotics, more patients will die from previously treatable infections. A key issue is how the value of antibiotics can be appropriately assessed by payers…

Incentives for New Drugs and Vaccines to Tackle Anti-Microbial Resistance
16 May 2017
Resistance to antibiotics is growing. Additional R&D is required. Both Transferable Intellectual Property Rights and Market Entry Rewards should be explored for use in Europe as…
Antimicrobials Resistance: A Call for Multi-disciplinary Action. How Can HTA Help?
1 October 2017
This briefing provides a detailed summary of a symposium held at the HTAi 2017 meeting in Rome. This briefing provides a detailed summary of a symposium…

Additional Elements of Value for Health Technology Assessment Decisions
1 May 2017
Antimicrobial resistance (AMR) occurs when microorganisms such as bacteria, viruses, fungi and parasites change in ways that render the medications used to cure the infections they…
Incentives for New Drugs to Tackle Anti-Microbial Resistance
1 May 2017
Resistance to antibiotics is growing, posing a major health risk in rich and poor countries. Additional ways of rewarding R&D are required. Mechanisms designed to encourage…

The Precautionary Principle in Healthcare
15 June 2016
In our daily lives, we take precautions routinely: we look both ways before we cross a road, and if we drive a car, we are constantly…
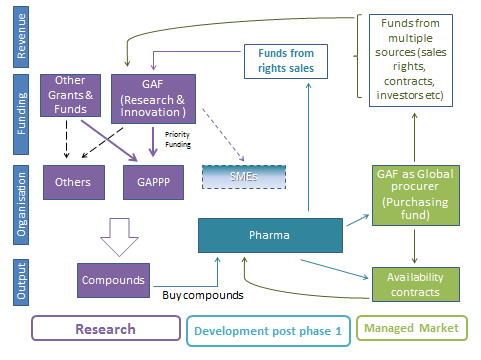
New Business Models for Antibiotics. What Can We Learn from Other Industries?
7 April 2015
The business model for antibiotics is broken. We looked at other industries facing conceptually similar challenges – particularly when the incentive for R&D is delinked from…

Spotlight on OHE: Innovation, Regulation and Antibiotics
30 September 2014
OHE long has been involved in analysing the nature of innovation and the effects of regulation. Two recent OHE presentations address the core issues.