Unlocking the Value of Combination Therapies



2024 Annual Lecture
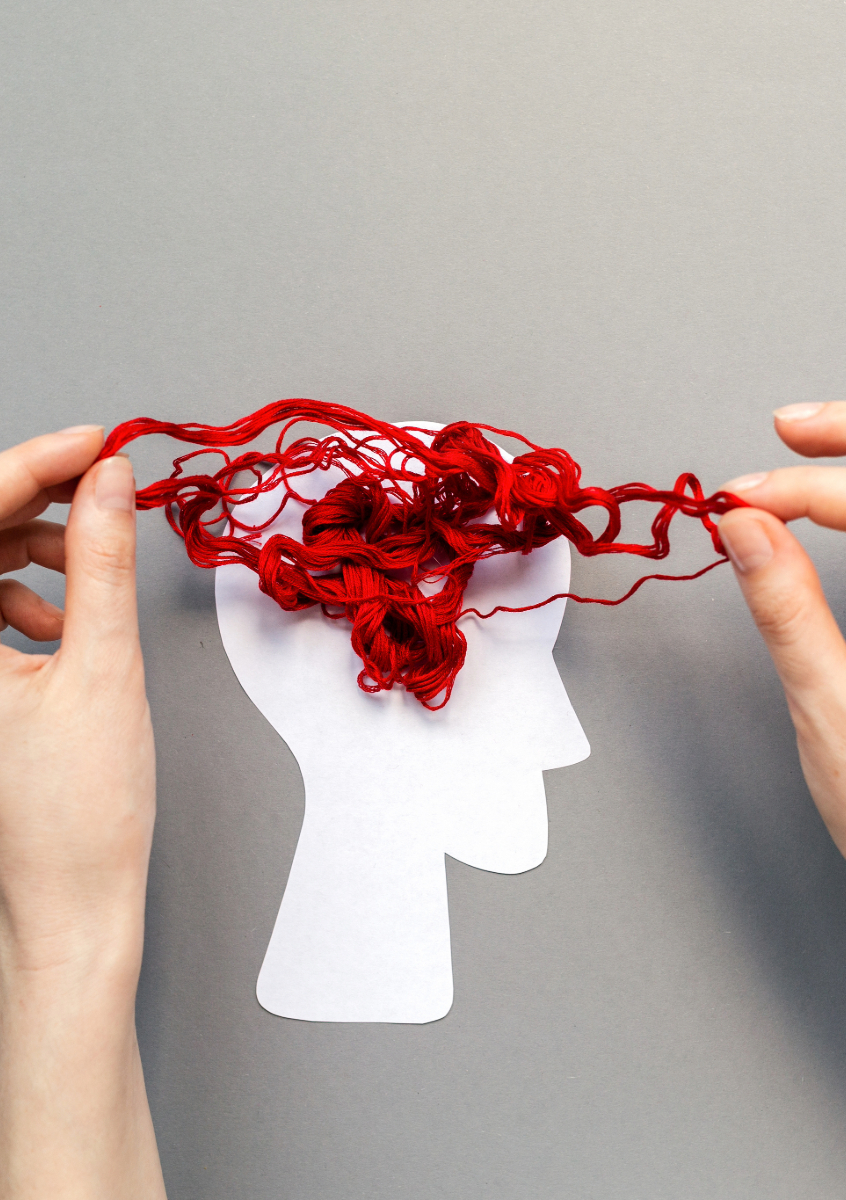
In this lecture, Professor Andrew Scott will re-evaluate prominent perceptions of ageing and argue for the need to focus on a longevity society and explore the key role of prevention in unlocking longer and healthier lives.
In the face of a healthcare crisis, the need to shift our focus from illness care to health care by enhancing our preparedness to prevent rather than to react is imperative, both for individual welfare and also economic strength. Professor Scott will outline the critical changes needed for society, the economy, and the health sector in particular for this paradigm shift to become a new reality where our society doesn’t just live longer, but also lives better.
The lecture is free to attend and will be followed by a Q&A session and a drinks reception.

About our Keynote Speaker
Andrew Scott is a Professor of Economics at London Business School, has worked extensively on the economics of longevity using a farsighted, multi-disciplinary approach. His latest book, “The Longevity Imperative – Building a Better Society for Healthier, Longer Lives”, is a convincing examination of the socio-economic consequences of humans living longer lives and the importance of adapting and adjusting to the reality of longer lives.
Register to attend in-person
OHE Annual Lecture Series
As part of our charitable purpose to educate and inform health policymakers, the Annual Lecture is our opportunity to highlight urgent and important issues facing health systems around the world and to raise awareness of research and evidence that can contribute to addressing these challenges. Throughout our long history we’ve had the privilege of hosting some of the greatest thinkers in the economics of health and health care.
An error has occurred, please try again later.
This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
Strictly Necessary Cookie should be enabled at all times so that we can save your preferences for cookie settings.
If you disable this cookie, we will not be able to save your preferences. This means that every time you visit this website you will need to enable or disable cookies again.
This website uses Google Analytics to collect anonymous information such as the number of visitors to the site, and the most popular pages.
Keeping this cookie enabled helps us to improve our website.
Please enable Strictly Necessary Cookies first so that we can save your preferences!